Contraceptives are a tricky topic. Not because it’s a taboo topic (is it?), but because there is not much research around it. There is not much research around it because research in this area is very time consuming and expensive.
This is what we know, in general, up to date:
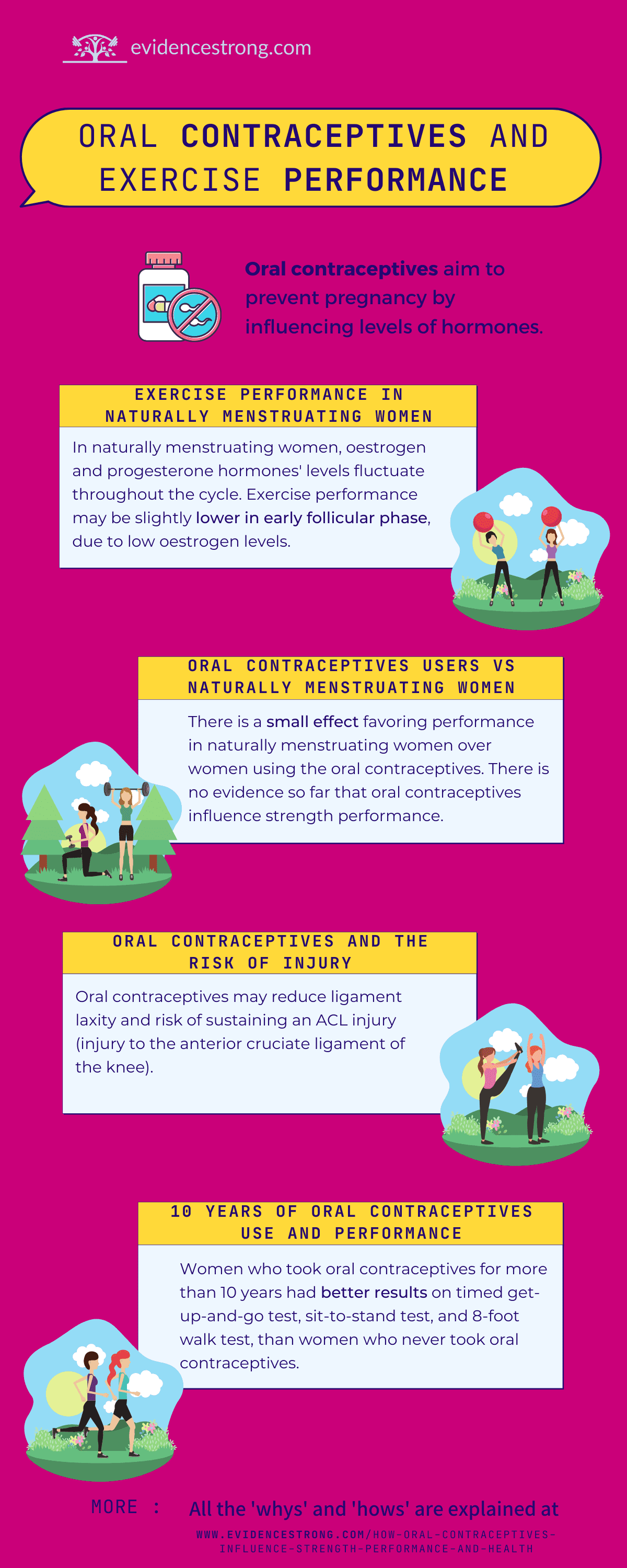
There is no evidence so far that oral contraceptives influence strength performance.
But this is in general, on average, or statistically speaking.
But human bodies, females included, are complicated. As you will soon learn, the research we have available can definitely indicate how contraceptives will influence you, but it cannot say for sure.
There are some aspects you can consider and use the available research to find the answer most likely to be applicable to YOU. Let’s start with how female hormones work in relation to strength in healthy, regularly menstruating women.
Normal menstrual cycle and exercise performance
First things first, let’s look at how a “typical” menstrual cycle works. The whole point of the menstrual cycle is to allow for pregnancy (having a baby). So all these changes are to prepare the female body to potentially grow a baby, then reset, and prepare again, it truly is a cycle. These changes in the body are controlled by hormones. The two hormones important for the menstrual cycle are oestrogen and progesterone.
Oestrogen and progesterone hormone levels fluctuate throughout the cycle:
- period starts in early follicular phase: low oestrogen and low progesterone
- late follicular: high oestrogen but low progesterone
- ovulation
- early luteal
- mid-luteal: high oestrogen and high progesterone
- late luteal
A review summarising results of 51 studies (362 comparisons: 240 for strength outcomes specifically). There was a trivial negative effect of early follicular phase which means that the exercise performance on average was slightly lower during the period.
Please keep in mind that there was a considerable variance between the studies and most of them were of low quality which means that different people can experience different reduction in performance or no reduction at all. This reduction is probably meaningless for most, but the elite athletes.
Why early follicular phase may reduce exercise performance?
Early follicular phase is the phase when both oestrogen and progesterone levels are low. Oestrogen has an anabolic (better glycogen usage), neuroexcitatory (easier to give best effort) and antioxidant (lower muscle damage and inflammation) effect. So all the advantages you want from your body when performing strength exercises.
In the early follicular phase, your body is not investing in producing much oestrogen and for that reason the performance may be reduced in some women. It makes sense when we go back to the very reason this cycle exists. Theoretically, when you have your period, you do not need to perform. Your body is resetting to then start preparing for the pregnancy.
When is the best time during the menstrual cycle to exercise then?
What a great question! If performance is low when oestrogen is low, then it would make sense that it is high when the oestrogen is high. Let’s talk about when the oestrogen is at it’s high.
During the cycle, oestrogen rises in the late follicular phase (right before the ovulation, which is in the middle of the cycle). This is also the time when progesterone is low. This high - low situation is important.
Progesterone is thought to have an anti-oestrogenic effect; it cancels the benefits of oestrogen. So the advantageous effects of oestrogen will potentially be the highest in the late follicular phase when the oestrogen is high but progesterone is low. Late follicular phase is just before ovulation, which is an opportunity for pregnancy. Therefore, it makes sense that physical performance will be potentially the highest in the late follicular phase.
The second peak in oestrogen is observed in mid-luteal phase (after ovulation), but it is also the time when progesterone (providing an anti-oestrogenic effect) is high. For that reason, the performance may not be as enhanced in the mid-luteal phase.
It is important to remember that the differences in performance caused by the menstrual cycle are small and probably matter only for the highest level athletes. On the other hand, variance was shown to be high in the studies which means that in a given population of women, the outcomes may differ substantially from one person to another. One person may experience no difference, another may experience a huge difference.
Oral contraceptives and exercise performance
Comparing oral contraceptive users with naturally menstruating women
Let’s look now at the research comparing exercise performance of naturally menstruating women with women who take oral contraceptives.
There is a small effect favoring performance in naturally menstruating women over women using the oral contraceptives. This conclusion was based on the outcomes pooled from 42 studies. But again, the variance in the performance results was considerable in these studies.
Why naturally menstruating women have better performance than oral contraceptive users?
In essence, oral contraceptives change hormonal levels in women’s bodies, this is how they prevent pregnancy. At the same time, the same hormone changes can potentially influence exercise performance (although usually very little).
In general, oral contraceptives down-regulate internal production (stop your body from producing) hormones, especially in the mid-luteal phase of the menstrual cycle (normally the phase when oestrogen and progesterone are high) and late-follicular phase (when normally oestrogen is high).
As a result, a woman who takes oral contraceptives displays a hormonal profile similar to the early follicular phase of a naturally menstruating woman (low oestrogen and low progesterone) all the time. For this reason, women who take oral contraceptives may be missing out on naturally occurring hormonal boost, especially in late follicular phase.
Do oral contraceptives influence a risk of injury in sports?
There is not much research on this topic. But from the research we have, we learned that oral contraceptives may reduce ligament laxity, and they also reduce a risk of sustaining an ACL injury (injury to the anterior cruciate ligament of the knee).
ACL injury is a huge problem in female sports as women athletes experience it 2-4 more often than their men counterparts. Should contraceptives be recognised as a strategy to reduce a risk of ACL injury in female athletes? We don’t know yet. We need more research.
How long-term use of oral contraceptives influences exercise performance and health?
So far we have looked at how taking oral contraceptives influences (or not) your performance at the time you are taking them. What about taking oral contraceptives for a long time, will it change your performance or health? Also, how taking contraceptives when young will affect women’s health later in life?
Long-term (10 years) oral contraceptives use and exercise performance
Post-menopausal women who took oral contraceptives for more than 10 years had better results on timed get-up-and-go test, sit-to-stand test, and 8-foot walk test, than women who never took oral contraceptives. These tests measure how fast a person can perform a task like standing up and walking. This means that long-term use of oral contraceptives can positively influence exercise performance later in life.
I have not found a study looking specifically into strength in postmenopausal women using contraceptives (if you find one, please send it my way).
Long-term oral contraceptives use and health
Oral contraceptives negatively influence cardiovascular health. Oral contraceptives increase risk of arterial events (e.g. myocardial infarction, ischemic stroke) and venous thromboembolism (e.g. deep vein thrombosis, pulmonary embolism). How high the risk is depends on the dose of the ethinylestradiol and type of progesterone used in the pill.
Another negative aspect of oral contraceptives use is an increased risk for breast and cervical cancer in women who are current or have been recently taking oral contraceptives, but this risk is lost within 5 years of stopping.
There are also some long-term health benefits to taking oral contraceptives. A study observing 23 thousand women for up to 44 years, has shown that women who have ever used combined oral contraceptives had lower risk of colorectal, endometrial and ovarian cancers even years after stopping (for at least 30 years) when compared to women who have never used oral contraceptives.
All right, the last thing: how oral contraceptives affect bone density?
One study looking at mostly post-menopausal women who were taking oral contraceptives for more than 10 years, have found that their bone density was higher than in women who didn’t take contraceptives. Also, women who were taking contraceptives earlier in life for 5 to 10 years, had less deformities in their spine after menopause.
Another study has found no effect in bone density between women who have taken oral contraceptives (even for more than 10 years) and women who have never taken oral contraceptives. As the results on influence of oral contraceptives on bone health are conflicting, I think we need to wait a bit longer for a definite answer. Close look at the dosage of hormones in oral contraceptives may offer some answers as the research emerges.
What does this all mean for you?
None of the research cited here has been done on you though.
In research we have, women who were taking contraceptives and the ones who didn’t were often very different in health-related and socioeconomic aspects. Also, the variance of effect of using contraceptives was big which means that different women had quite different results. You can definitely use this research as your starting point but there are other things you can consider.
To make an informed decision on what is best for you, you should look at your family history (e.g. did the women in your family have any circulatory (cardiovascular) problems), what are your personal health risks, what are your goals as an athlete, and perhaps talk to the health professional you trust.
Please take care of your health, Alex
Readings
Allali F, El Mansouri L, zohra Abourazzak F, Ichchou L, Khazzani H, Bennani L, Abouqal R, Hajjaj-Hassouni N. The effect of past use of oral contraceptive on bone mineral density, bone biochemical markers and muscle strength in healthy pre and post menopausal women. BMC women’s health. 2009 Dec;9(1):1-6.
Elliott-Sale KJ, McNulty KL, Ansdell P, Goodall S, Hicks KM, Thomas K, Swinton PA, Dolan E. The effects of oral contraceptives on exercise performance in women: a systematic review and meta-analysis. Sports medicine. 2020 Jul 14:1-28.
Iversen L, Sivasubramaniam S, Lee AJ, Fielding S, Hannaford PC. Lifetime cancer risk and combined oral contraceptives: the Royal College of General Practitioners’ Oral Contraception Study. American journal of obstetrics and gynecology. 2017 Jun 1;216(6):580-e1.
Konopka JA, Hsue LJ and Dragoo JL. Effect of oral contraceptives on soft tissue injury risk, soft tissue laxity, and muscle strength: a systematic review of the literature. Orthopaedic journal of sports medicine. 2019 7(3); p.2325967119831061.
McNulty KL, Elliott-Sale KJ, Dolan E, Swinton PA, Ansdell P, Goodall S, Thomas K, Hicks KM. The effects of menstrual cycle phase on exercise performance in eumenorrheic women: a systematic review and meta-analysis. Sports medicine. 2020 Jul 13:1-5.
Oedingen C, Scholz S, Razum O. Systematic review and meta-analysis of the association of combined oral contraceptives on the risk of venous thromboembolism: the role of the progestogen type and estrogen dose. Thrombosis research. 2018 May 1;165:68-78.
Wei S, Venn A, Ding C, Foley S, Laslett L, Jones G. The association between oral contraceptive use, bone mineral density and fractures in women aged 50–80 years. Contraception. 2011 Oct 1;84(4):357-62.